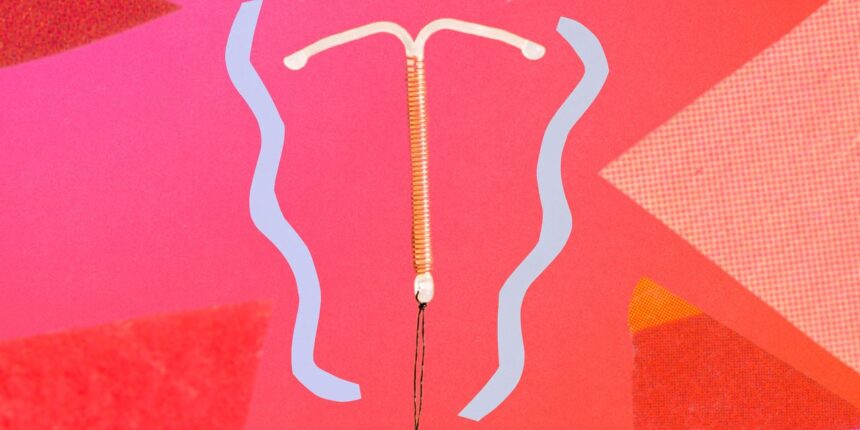
Last week, the American College of Obstetricians and Gynecologists (ACOG) acknowledged in writing what people with a uterus have shouted from the rooftops for years: In-office gynecological procedures, like intrauterine device (IUD) insertions or cervical biopsies, can be far more agonizing than the “pinch” often promised. The org published new guidelines on May 15 calling on doctors to “not underestimate” this pain and instead offer patients evidence-based options for managing it. It’s overdue, yes—but it also paves the way for patients to advocate for themselves and actually be taken seriously.
One of the biggest changes in this document, though it may seem trivial, is the push for doctors to talk to patients about pain management in these contexts in the first place, Eve Espey, MD, MPH, chair of the obstetrics and gynecology department at the University of New Mexico, tells SELF. It builds on CDC recommendations released last fall (on pain management for IUD insertion, specifically), which were the first to urge doctors to routinely have this kind of convo.
If you’re wondering what took so long, part of the reason it’s been so commonly skipped boils down to implicit bias: Research shows providers more readily dismiss women’s pain and Black women’s pain in particular. Logistics may also play a role, Dr. Espey says. There can be so much for your doctor to go over in a short appointment: They need to explain the risks of the procedure, for instance, and what to expect afterward, so the issue of pain during the operation may have fallen by the wayside. The new ACOG guidance, by contrast, encourages doctors to recognize what a big deal the procedure itself can be to patients and treat it as such, Dr. Espey says.
Another reason why doctors may have hesitated to discuss pain control for gyno procedures? Pain is tricky to study because of its subjectivity (not to mention, women’s health is underfunded in general), so there’s not as much conclusive research on the available options as many would prefer, Rachel Blake, MD, FACOG, a board-certified ob-gyn in New Jersey, tells SELF. But the new guidelines suggest there’s now enough data to recommend certain types of pain management for particular procedures, Dr. Blake says. The consensus is that, given how miserable these surgeries can be for some people, it’s well worth it for doctors to at least present these relief options and give patients the autonomy to choose whether they’ll use them.
As with any new medical guidance, though, it may take some time for this kind of care to be incorporated into standard practice, Dr. Blake notes. If your ob-gyn doesn’t bring up pain control when talking through an upcoming procedure, here’s how to broach the topic and weigh your options to make it as manageable as possible.
1. Feel empowered to ask about pain directly.
The exciting thing about not one but two large orgs coming out with guidelines about gynecological pain in recent months is that it lends a lot of credence to the issue. It’s tougher for your doctor to wave away your concerns when both the CDC and ACOG have recommended they address them. Dr. Espey suggests simply posing the question: “I’ve heard this is a painful procedure. Can you let me know what options are available to address the discomfort that I think I’m going to feel with this?”
Read the full article here